Should You Be Taking Probiotics With Antibiotics?
Since 1929, when scientist Alex Fleming discovered penicillin, antibiotics have saved millions of people from severe illnesses and infections. While there is no denying the necessity of antibiotic use in modern medicine, if you’re like me, you can’t help but shudder slightly when your doctor prescribes an antibiotic to resolve your health issue.
“Each time I’ve asked my doctor about taking probiotics alongside the meds to ward off the dreaded gut imbalance and side effects, it feels like I hear a different opinion.”
Having endured chronic ear infections as a child, I was on a constant dose of the bubble gum-flavored pink goo — aka amoxicillin. Because of this, I am all too aware of the side effects of antibiotics — mainly belly aches and long-term disruption to gut health. As an adult, I’ve thankfully only needed antibiotics a handful of times, and the same when it comes to my daughters. But each time I’ve asked my doctor or their pediatrician about taking probiotics alongside the meds to ward off the dreaded gut imbalance and side effects, it feels like I hear a different opinion. So what is the deal?
While the evidence does confirm that probiotics are beneficial during antibiotic use, there still needs to be more consensus in a clinical setting regarding how much they help and how best to take them.
“We still don’t know the dosage, frequency, length of intervention, and bacteria composition that would be most beneficial for probiotic interventions during antibiotic treatment. Therefore a lot more research in the area is highly needed.” Dr. Elisa Marroquín, author of a study on probiotic use with antibiotics, told Medical News Today.
We’ve done some of our own research and laid out our findings regarding taking probiotics with antibiotics, including when, how, and what probiotics to consider.
Why take probiotics with antibiotics?
Alongside the advancements in antibiotic therapies, the role of a healthy and balanced microbiome has also been at the forefront of health goals. A healthy microbiome offers benefits like increased immunity against infection and harmful pathogens, better digestion, and optimal absorption of nutrients. We now know that antibiotics can negatively affect that balance, killing good and bad bacteria, leading to internal flora imbalances, and causing side effects like tummy troubles and secondary infections. Enter probiotics.
“A healthy microbiome offers benefits like increased immunity against infection and harmful pathogens, better digestion, and optimal absorption of nutrients.”
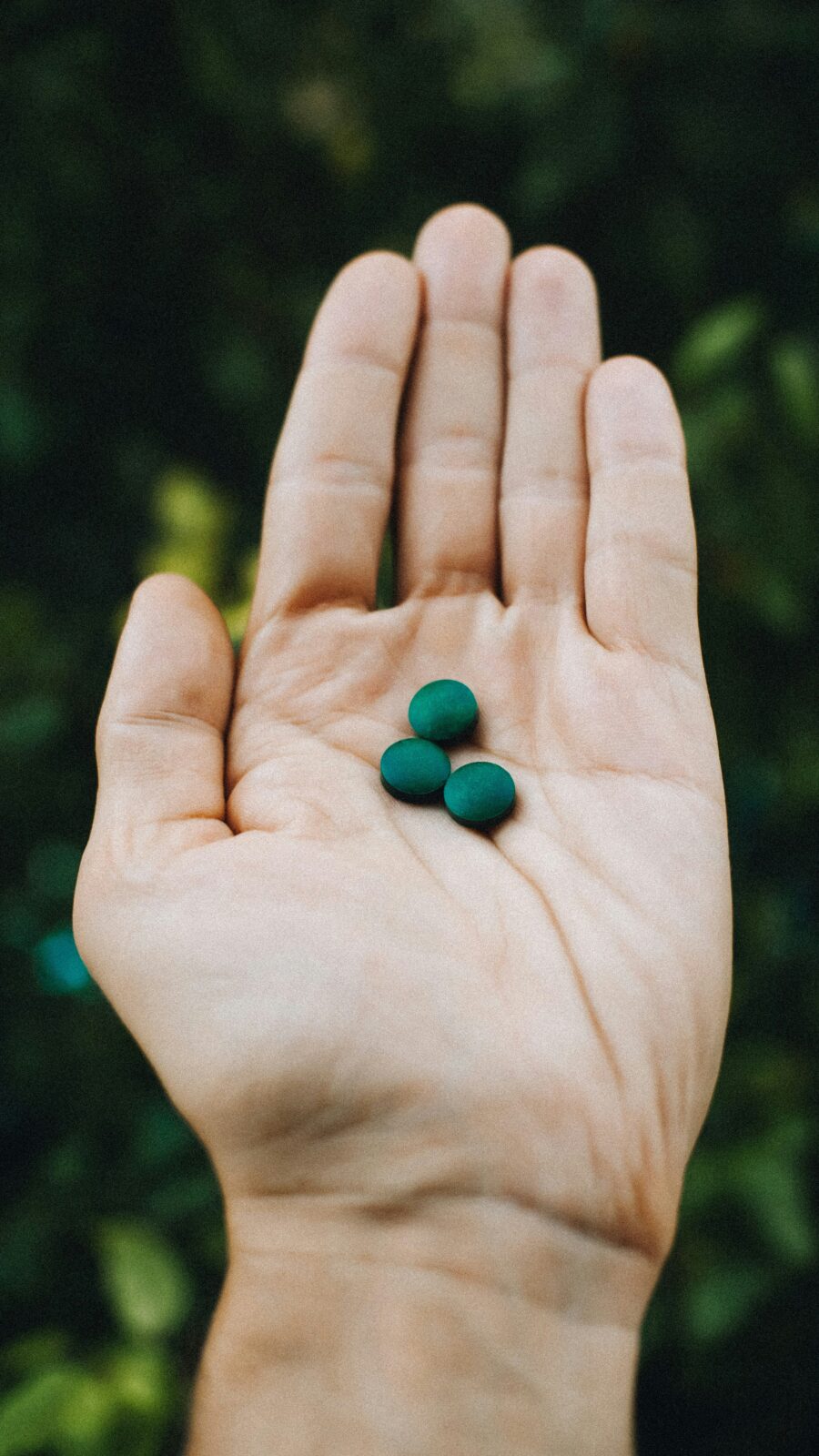
Whether delivered through the food you consume or dietary supplementation, probiotics are essentially touted as the superheroes of the bacteria world — providing beneficial microbes that keep malicious bacteria in check while simultaneously optimizing internal flora.
Although probiotics may seem like the key to restoring gut microbiome diversity thrown off by antibiotic use, one study found that probiotics don’t exactly work that way. That’s not to say you should discount the role of probiotics while taking antibiotics.
The American Gastroenterological Association still suggests taking specific probiotics alongside antibiotics to dodge or mitigate nasty side effects like antibiotic-induced diarrhea and a dangerous infection known as C-Difficile. There is also some evidence that probiotics can make antibiotics more effective, like in the case of patients with H Pylori. And mounting evidence shows that probiotics taken with a course of antibiotics used to treat pesky bacterial vaginosis (BV) can help prevent infection recurrence. However, not all probiotics are the same, and considerations should be made to determine which probiotic is best and how to take it.
How to take probiotics with antibiotics
Unfortunately, there is no written rule on how best to take a probiotic when on antibiotics. But if you’ve been advised to take a probiotic during a course of antibiotics, the timing in which you take them in relation to the time you take your medicine may play a role in the effectiveness of both. What seems to be a standard recommendation from healthcare providers is to separate the consumption of your antibiotic and your probiotics by at least 1–2 hours. We also found recommendations that suggested closer to 4–6 hours.
“For the most protection against antibiotic-induced diarrhea, evidence suggests starting a probiotic as early as possible during your course of antibiotics.”
Also, for the most protection against antibiotic-induced diarrhea, evidence suggests starting a probiotic as early as possible during your course of antibiotics — within 1 to 2 days is ideal. Whether or not to continue your probiotic after treatment is contentious; however, one study suggests continuing a probiotic a week after completing antibiotics. In contrast, other research says continuing probiotics post-antibiotic might delay overall gut health recovery.
What probiotics should you take with antibiotics?
The strain of probiotics you take also holds weight, as certain probiotics have undergone testing to ensure viability alongside antibiotics. Taking non-recommended probiotics may be a waste of money as the antibiotic could kill them without letting the probiotic do its job. And, while still generally safe for most, when the incorrect probiotic strain is taken for a condition, it can exacerbate the issue or cause side effects like gas and bloating.
“Taking non-recommended probiotics may be a waste of money as the antibiotic could kill them without letting the probiotic do its job.”
When using a probiotic to combat the side effects of antibiotics, it’s best to stick to researched strains or strain combinations found to be most effective alongside antibiotics. Four probiotics recommended for use with antibiotics and that continuously come up in research are:
- Lactobacillus rhamnosus GG
- Bifidobacterium animalis SPP lactis (BB12®)
- Saccharomyces boulardii
- Lactobacillus acidophilus
You can find many of these in over-the-counter probiotic brands — but we recommend considering your general health, your response to medications and probiotics, and consulting a professional before you decide what course to take.
Why don’t all doctors prescribe probiotics with antibiotics?
This is a tricky question! And again, there is no straightforward answer. Doctors may be hesitant about recommending probiotics while taking antibiotics for several reasons. First, there is constantly conflicting information and studies on probiotic effectiveness, not to mention no clinical consensus on how best to take them. Second, for the most part, there is no accurate regulation of probiotics. That means when a patient purchases probiotics, there is no way to know exactly how much they are getting or the quality of the product. Third, some patients may be at health risk from taking probiotics. While this is a tiny portion of the population, it can’t be discounted as no risk.
“Consult with your doctor first and then stick with their recommended brands of probiotics for use alongside antibiotics.”
There is compelling evidence that taking the right strain of probiotics during antibiotic therapy can help prevent antibiotic-induced side effects, specifically digestive issues. However, the research needs to be clarified! We still don’t know if probiotics have a positive broader benefit for use alongside antibiotics. Although some still suggest probiotics can help repopulate the gut with good bacteria and repair the imbalance caused by antibiotics, there is not enough proof. And some studies even contradict this.
Regarding probiotic use, it still seems best to consult with your doctor first and then stick with their recommended brands of probiotics for use alongside antibiotics. Next time you’re stuck on a course of antibiotics, use the information above to help formulate your question. Let us know how it goes!
Randi Donahue is a Contributing Editor at The Good Trade. She is a freelance writer who lives on the Gulf Coast of Florida and is fortunate to live right next to a glorious nature preserve and a few miles from a white sandy beach. She and her family are passionate about nature, health & wellness, and sustainable living and believe the path to a healthy and prosperous life requires authenticity, kindness, and a whole lot of fresh air.




